One of my patients, who also is a doctor, sent me this article from a website known as “The Medical Republic” with the title “Coronary artery calcium scoring provides no clinical benefit.” This was based on a systematic review published in JAMA Internal Medicine (1), with the initial paragraph after the introduction stating “that while the scans might provide some additional information beyond traditional risk factors, it was unclear whether this translated into fewer heart attacks and strokes for people who took the test.”
The lead author was associate Professor Katy Bell from Sydney University and when interviewed stated that coronary calcium scans created the risk of over-diagnosis and over-treatment in some patients.
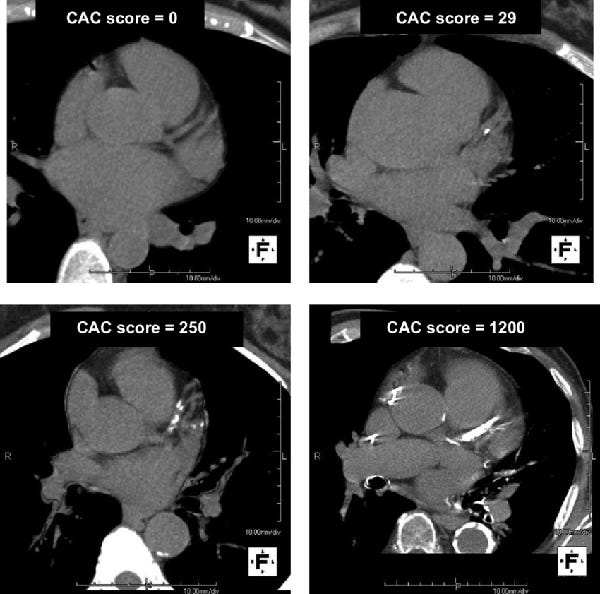
The author of this article then quoted me as a vocal proponent of coronary calcium scans and reported accurately from an article I wrote for “Switzer Daily” where I stated that “coronary artery calcium scoring (only in patients without a prior history of heart disease) is the most accurate predictor of cardiac risk. Coronary calcium scoring provides a picture of the coronary arteries, which is a surrogate marker for the accumulation of fat in the arteries over decades up to the point of scanning. The great value of coronary artery calcium scoring is that it is quantitative i.e. the higher the calcium score, the higher the risk.
The article then went on to suggest that attempts by TMR to contact Dr. Walker to discuss the JAMA research were unsuccessful.
The only attempt made to contact me was a Facebook message sent to me over the Easter break and, as I was on holidays, I missed the message.
As I am a vocal proponent of coronary calcium scoring and also the person who introduced this test into Australia in 1999, in conjunction with the Sydney Adventist Hospital and Dr. David Grout, one of my cardiology colleagues, I felt it important to address the very flawed conclusions from this study and the biased bent of this article.
This study was a pooled meta-analysis of cohort studies in primary prevention using the combination of standard cardiac risk calculators which include assessment of cholesterol, blood pressure, cigarette smoking, diabetic risk and family history and then determined the incremental benefit of coronary calcium scoring.
The basic function of a coronary calcium score is to classify a person as either low, medium or high risk. The obvious flaw of this study is that shifting a person from one category to another then changes management.
If you are considered high risk because of the number of risk factors for heart disease but have a zero or very low coronary calcium score then you typically do not require pharmaceutical therapy to manage cholesterol. This saves a number of patients being exposed to potential side effects of drugs over many years and that is the extraordinary benefit of coronary calcium scoring, but also to mention the reassurance that you are at very low risk for an event.
If, however, you are initially deemed as being at low risk but the coronary calcium score suggests you are at high-risk, then you may require long-term pharmaceutical therapy in conjunction with a healthy lifestyle to control your cardiovascular risk.
All this particular study shows is that knowing your true risk with a combination of standard risk factors and coronary calcium scoring markedly reduces your risk for further cardiovascular events regardless of what group you were in, because of the appropriate use of therapy, based on risk category. Thus, the incremental benefit from coronary calcium scoring.
As it is unethical to avoid aggressive management of risk factors in high-risk individuals, this study purely reinforces that doing so works!
There have been numerous studies to show that once a doctor knows a person’s coronary calcium score, they are much more aggressive with their risk factor modification if the person is at high risk. Once a patient knows they have a significant amount of coronary calcium, they are much more diligent with lifestyle modification as well.
There has also been a large study of 13,500 patients, in people over the age of 50, followed for 10 years demonstrating that if your coronary calcium score is below 100, there is no value in taking statin therapy. If your coronary calcium score is above 100, however, this is where the value of statins is proven.
Therefore, regardless of the very flawed conclusions from this study, I will continue to suggest that all males at 50 and all females at 60 without a history of existing heart disease should have a coronary calcium score as this will determine firstly their risk over the next 5 to 10 years and also the need for pharmaceutical therapy based on the coronary calcium score.
High cholesterol is being over-treated in many people and the only way to determine whether taking a statin is necessary is to have a coronary calcium score. Articles such as that written by The Medical Republic, not analysing the true implications of the JAMA study are very unhelpful and confusing for the public who do not understand this area.
I was quoted correctly by The Medical Republic when I said that the best treatment of all modern disease is to not get them in the first place i.e. prevention. The first step in prevention of heart disease is to know your level of risk. The most accurate level risk predictor is, no doubt, coronary calcium scoring.
1) April 25, 2022
Evaluation of the Incremental Value of a Coronary Artery Calcium Score Beyond Traditional Cardiovascular Risk Assessment: A Systematic Review and Meta-analysis
Katy J. L. Bell, PhD1; Sam White, MD1; Omar Hassan, MD1; et al
Dr Walker is a consultant cardiologist who is not financially associated with any coronary calcium scoring service & therefore has no disclosures in this regard.